Streptococcus pneumoniae is a normal inhabitant of the human
upper respiratory tract. The bacterium can cause pneumonia, usually of
the lobar type, paranasal sinusitis and otitis media, or meningitis,
which
is usually secondary to one of the former infections. It also
causes osteomyelitis, septic
arthritis, endocarditis, peritonitis, cellulitis and brain abscesses. Streptococcus
pneumoniae is currently the leading cause of invasive bacterial
disease
in children and the elderly. Streptococcus
pneumoniae is known in medical microbiology as the pneumococcus,
referring to its morphology and its consistent involvement in
pneumococcal
pneumonia.
Pneumonia is a disease of the lung that is
caused by a variety
of bacteria including Streptococcus, Staphylococcus, Pseudomonas,
Haemophilus,
Chlamydia and Mycoplasma, several viruses, and certain fungi and
protozoans. The disease may be divided into two forms, bronchial
pneumonia
and lobar pneumonia. Bronchial pneumonia is most prevalent in infants,
young children and aged adults. It is caused by various bacteria,
including
Streptococcus
pneumoniae. Bronchial pneumonia involves the alveoli contiguous to
the larger bronchioles of the bronchial tree. Lobar pneumonia is more
prone
to occur in younger adults. A majority (more than 80%) of the cases of
lobar pneumonia are caused by Streptococcus pneumoniae. Lobar
pneumonia
involves all of a single lobe of the lungs (although more than one lobe
may be involved), wherein the entire area of involvement tends to
become
a consolidated mass, in contrast to the spongy texture of normal lung
tissue.
Bacteriology
Streptococcus pneumoniae cells are Gram-positive,
lancet-shaped cocci
(elongated cocci with a slightly pointed outer curvature). Usually,
they
are seen as pairs of cocci (diplococci), but they may also occur singly
and in short chains. When cultured on blood agar, they are alpha
hemolytic. Individual cells are between 0.5 and 1.25 micrometers in
diameter. They
do not form spores, and they are nonmotile. Like other streptococci,
they
lack catalase and ferment glucose to lactic acid. Unlike other
streptococci,
they do not display an M protein, they hydrolyze inulin, and their cell
wall composition is characteristic both in terms of their peptidoglycan
and their teichoic acid.
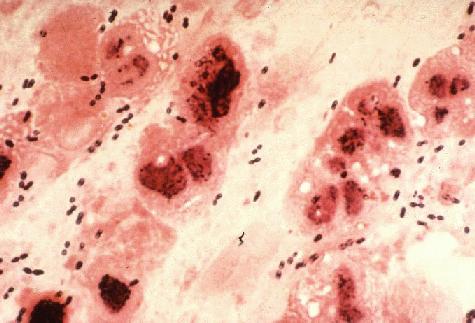
Gram Stain of a film of sputum
from a case of lobar pneumonia. CDC.
Cultivation
Streptococcus pneumoniae is a fastidious bacterium, growing
best
in 5% carbon dioxide. Nearly 20% of fresh clinical isolates require
fully
anaerobic conditions. In all cases, growth requires a source of
catalase
(e.g. blood) to neutralize the large amount of hydrogen peroxide
produced
by the bacteria. In complex media containing blood, at
37°C,
the bacterium has a doubling time of 20-30 minutes.
On agar, pneumococci grow as glistening colonies, about 1 mm
in
diameter. Two serotypes, types 3 and 37, are mucoid. Pneumococci
spontaneously
undergo a genetically determined, phase variation from opaque to
transparent
colonies at a rate of 1 in 105 . The transparent colony type
is adapted to colonization of the nasopharynx, whereas the opaque
variant
is suited for survival in blood. The chemical basis for the difference
in colony appearance is not known, but significant difference in
surface
protein expression between the two types has been shown.
Streptococcus pneumoniae is a fermentative aerotolerant
anaerobe.
It is usually cultured in media that contain blood. On blood agar,
colonies
characteristically produce a zone of alpha (green) hemolysis, which
differentiates
S.
pneumoniae from the group A (beta hemolytic) streptococcus,
but
not from commensal alpha hemolytic (viridans) streptococci which are
co-inhabitants
of the upper respiratory tract. Special tests such as inulin
fermentation,
bile solubility, and optochin (an antibiotic) sensitivity must be
routinely
employed to differentiate the pneumococcus from Streptococcus
viridans.

Streptococcus pneumoniae
Gram-stain
of blood broth culture. CDC.
Streptococcus pneumoniae is a very fragile bacterium and
contains
within itself the enzymatic ability to disrupt and to disintegrate the
cells. The enzyme responsible is called an autolysin. The
physiological
role
of this autolysin is to cause the culture to undergo a characteristic
autolysis
that kills the entire culture when grown to stationary phase. Virtually
all clinical isolates of pneumococci harbor this autolysin and undergo
lysis usually beginning between 18-24 hours after initiation of growth
under optimal conditions. Autolysis is consistent with changes in
colony morphology. Colonies initially appear with a plateau-type
morphology,
then start to collapse in the centers when autolysis begins.
Identification
The minimum criteria for identification and distinction of
pneumococci
from other streptococci are bile or optochin sensitivity, Gram-positive
staining, and hemolytic activity. Pneumococci cause alpha hemolysis on
agar containing horse, human, rabbit and sheep erythrocytes. Under
anaerobic
conditions they switch to beta hemolysis caused by an oxygen-labile
hemolysin.
Typically, pneumococci form a 16-mm zone of inhibition around a 5 mg
optochin
disc, and undergo lysis by bile salts (e.g. deoxycholate). Addition of
a few drops of 10% deoxycholate at 37°C lyses the entire culture in
minutes. The ability of deoxycholate to dissolve the cell wall, depends
upon the presence of the autolytic enzyme, LytA. Virtually all clinical
isolates of pneumococci harbor the autolysin and undergo deoxycholate
lysis.

Streptococcus pneumoniae
A mucoid strain on blood agar showing alpha hemolysis (green zone
surrounding
colonies). Note the zone of inhibition around a filter paper disc
impregnated
with optochin. Viridans streptococci are not inhibited by optochin.
Serotyping
The quellung reaction (swelling reaction) forms the basis of
serotyping and relies on the swelling of the capsule upon binding of
homologous
antibody. The test consists of mixing a loopful of colony with
equal
quantity of specific antiserum and then examining microscopically
at 1000X for capsular swelling. Although generally highly specific,
cross-reactivity
has been observed between capsular types 2 and 5, 3 and 8, 7 and 18, 13
and 30, and with E. coli, Klebsiella, H. influenzae Type b, and
certain
viridans streptococci.

Streptococcus pneumoniae
Quellung (capsular swelling) reaction can be used to demonstrate the
presence
of a specific capsular type of the bacterium.
what is Streptococcus pneumoniae ??
Langganan:
Posting Komentar (Atom)




0 komentar:
Posting Komentar